Introduction
Eosinophils are a type of white blood cell that are part of the immune system and protect the body from allergens, parasites and other foreign organisms. They are proinflammatory cells that release enzymes and proteins when the body encounters a substance it wants to attack, such as an allergen or parasite. That’s why it wont be wrong to say Eosinophils are soldiers patrolling for invaders.
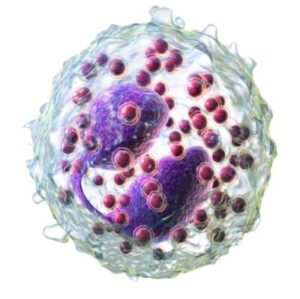
Structure of Eosinophils :-
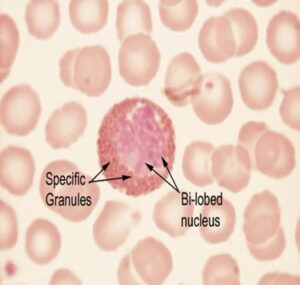
- Bilobed nucleus: The nucleus of an eosinophil is characteristically bilobed, resembling a horseshoe or spectacle shaped nucleus.
- Granules: Eosinophils contain eosinophilic large granules filled with proteins that are stained red by eosin dye, hence the name “eosinophil.”
- Major basic protein (MBP): One of the key proteins found in eosinophil granules is major basic protein (MBP), a potent toxin against parasites and some mammalian cells.
- Eosinophil cationic protein (ECP): Another important granule protein is eosinophil cationic protein (ECP), which also has cytotoxic activity against parasites and contributes to inflammation.
Function of Eosinophils :-
Phagocytosis: Eosinophils can engulf and destroy parasites, bacteria, and other foreign substances.
Cytotoxicity: Eosinophils can release toxic proteins that kill parasites and other cells.
Allergic reactions: Eosinophils can release chemicals that contribute to the development of allergic reactions, such as asthma and hay fever.
Inflammation: Eosinophils can release chemicals that contribute to the development of inflammation.
What is the formula for Absolute Eosinophil Count (AEC) :-
The formula for Absolute Eosinophil Count (AEC) is:
AEC = (WBC count) x (Eosinophil percentage) / 100Absolute Eosinophil count
Normal Range: 0-500 cells/mcL
(AEC) ≥ 500 cells/mcL is ABNORMAL; is called as eosinophilia.
Eosinophil is a predominantly tissue dwelling cell so eosinophil DON’T correlate with tissue damage 🤷♂️. That’s why we see few patients with increased Eosinophil and no heart & lung injury !!
Where do eosinophils come from?- Bone Marrow
They are cells of the granulocytic lineage, siblings of neutrophils & basophils, children of the myeloblast (image👇🏻) Eosinophil Biology.
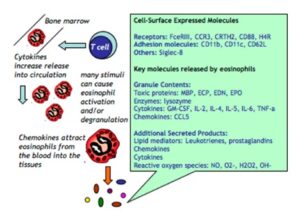
IL5 is the cytokine responsible for it’s production, important to know because anti IL5 monoclonal Antibody is available.
Why do we care absolute eosinophilia?
Eosinophils are GRANULAR cells and the granules contain toxic material.
⤴️Eos= ⤴️ degranulation= ⤴️toxic contents= 🫁🫀🧠damage !!
Let’s start with the clinical bit-
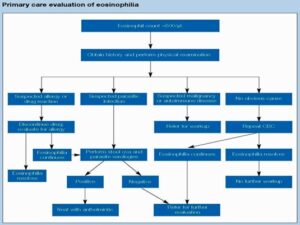
Approach for eosinophilia ?
Start with a CLINICAL HISTORY: Drug history is very IMPORTANT. Always ask about complementary drug intake. This could be recent or remote.
What are the other causes of eosinophilia?
- Allergies
- Parasitic infections
- Malignancies
- Auto-Immune disorders
- eosinophilic granulomatosis with polyangiitis (EGPA), and
- eosinophilic esophagitis.
Low AEC (Eosinopenia):
-
Acute infections: initial stages of an infection.
- Cushing’s syndrome: High levels of cortisol can suppress eosinophil counts.
- Stress: Physical or emotional stress can lead to a temporary decrease in eosinophils.
What organs are most often affected??
- Skin, Lungs, heart, Brain, GI tract
- Ask if the patient has a rash, cough, wheezing, palpitations, dyspnoea, diarrhoea etc.
- On examination, look for enlarged lymph nodes, liver and spleen!
- Always auscultate the Cardioplumonary system.
- If there’s something abnormal on the exam, it could be eosinophil related end organ damage
- PERSISTENT Increase in eosinophils (≥1500/mcL) AND end organ damage = HES (Hypereosinophilic syndrome).
- This could be due to any cause and HES ≠ malignancy all the time. i.e. the degree of ⤴️⤴️ ≠ malignant cause.
- HES is a syndrome, one has to find the underlying cause.
HES could be due to a myeloid neoplasm (M-HES), clonal lymphocytes (T-HES) or even be familial.
But most often our investigations don’t reveal anything and we are forced to call it “idiopathic” HES.
Why is it important to recognise the underlying cause??
- To treat and prognosticate better. M-HES for example is treated differently, it responds to imatinib and responds poorly to steroids.
- M-HES is due to a chromosomal rearrangement involving FIP1L1-PDGFRa, can be tested for by FISH.
- Also associated with ⤴️ vitamin B12 and ⤴️tryptase, most often with splenomegaly.
If you suspect this, call your hematologist!!
- More often than not, eosinophilia will be transient and secondary to drugs/infections. Will resolve with appropriate Rx and drug withdrawal.
What if it doesn’t ??
Let’s SUMMARISE
- Hypereosinophila ≥ 1500 cells/mcL
- HES is above + organ damage
- HES has many varieties, some are cancers
- MC organs involved 🫁♥️🧠, skin, GI tract
- Mostly transient, sec to infections/drugs
- If persistent, involve a hematologist
LABORATORY INVESTIGATIONS:
- Complete blood counts with peripheral blood smear exam esp. for parasites like microfilaria, stool examination for parasite detection, metabolic panel, infection screen, radiological investigation & Tissue biopsy wherever indicated.
- Additional Investigations depends on the symptoms and what the underlying suspected disease is.
- Think of M-HES in a young male with cardiac involvement, L-HES involves more of skin!
- EGPA will present with 🫁 findings so tests depend upon clinical suspicion.
- But we test with 2 things in mind, identifying the UNDERLYING CAUSE of HES and tests to IDENTIFY END ORGAN DAMAGE (eg. Troponins)
When do we treat URGENTLY ?
When there’s severe organ damage like respiratory distress, other cardiac & cerebral symptoms !
Admit and treat immediately.
Steroids are magical 🪄🪄🪄
- For most other situations, it’s ok to initiate traetment on an OPD basis.
- Starting steroids before establishing a diagnosis is tricky business, must be avoided. It can change everything. Tread very carefully!
- If someone urgently needs to reduce eosinophils, use hydroxyurea while awaiting the test results. Once the results are in, treat accordingly.
M-HES is treated with imatinib as imatinib blocks PDGFR in addition to BCR::ABL1. The dose used here is <<CML (100mg OD)
If M-HES has cardiac symptoms (usually does), start imatinib + steroids to avoid fatal myocardial infarction & necrosis.
- For all other HES variants, the treatment is CORTICOSTEROID 🪄🪄🪄
- The usual corticosteroid used is prednisone at 1 mg/kg.
- Some use higher doses of methylprednisolone like 1 gm/d x 3 days. Some use this dose only if severe symptoms or underlying autoimmune disease is the cause of HES.
How long to continue steroids??
- Literature & few physcians mention it to continue till AEC ≤ 1500 & till symptoms resolve and then taper.
- If the patient needs >10 mg steroids for the same, start a steroid sparing drug.
Which are those steroid sparing drugs?
- Hydroxyurea
- Interferon a
- Mepolizumab
Mepolizumab
- It is an anti IL-5 monoclonal antibody.
- IL5 is required for eosinophil production, so mepolizumab blocks
- Dosed at 300mg subcutaneous once a month. It is available in India but its expensive. Our options are hydroxyurea over IFNα.

SUMMARY
- Absolute Eosinophil count (AEC) ≥ 500 cells/mcL with organ damage = HES
- HES has many variants:
- Myeloid-HES treated differently from the rest (imatinib > steroids)
- All other HES variants are treated with corticosteroids initially followed by steroid sparing drugs if needed.
Very often the underlying cause won’t be identified = idiopathic HES.

Really instructive and fantastic complex body part of articles, now that’s user friendly (:.
Unquestionably believe that which you stated. Your favorite reason appeared to be on the web the easiest thing to be aware of. I say to you, I certainly get annoyed while people think about worries that they just don’t know about. You managed to hit the nail upon the top and defined out the whole thing without having side-effects , people could take a signal. Will probably be back to get more. Thanks